This occurs when the ventilator is not meeting the patient’s requirements resulting in a mismatch between the support the ventilator provides and the support that the patient wants.
The patient with dyssynchrony may present with distress, agitation, hypoxia, or the ventilator may alarm frequently with abnormal waveforms. Prolonged dyssynchrony may result in VILI. Assessment of dyssynchrony is very complex. This page is merely meant as an overview. Senior support should always be sought.
Causes are both ventilator settings and patient factors (these include high or low respiratory drive, inadequate sedation, weak inspiratory efforts, and intrinsic PEEP).
Working out the cause and adjusting the ventilator to meet the patient’s needs is much better than deepening the patient’s sedation to tolerate the chosen ventilatory settings. However, if there is an acute deterioration then the use of a sedative bolus +/- paralysis is not unreasonable.
Types of Ventilator Dyssynchrony
The types of dyssynchrony can be split into the different parts of the breath (see invasive ventilation page). This is not an exhaustive list.
Please note that some of the waveforms will look different depending on whether the patient is receiving volume or pressure ventilation.
- Trigger
- Too low or too high
- Flow dyssynchrony
- Often the demands of patient exceed the flow provided by the patient
- Cycling
- Too early or too late
- Others
- Alarm limits
- Review the alarms set on the ventilator
- If set too low and the parameters exceeds set limit it might result in termination of breath.
- e.g. if PIPs exceed set limit, breath terminated and delivered tidal volumes may be small; or if upper limit for tidal volume set too low then delivered tidal volume may be ceased at set volume. This will result in dyssynchrony if the patient desires larger tidal volumes than the ventilator is giving.
- Review the alarms set on the ventilator
- Management will revolve around either altering the alarm limit or considering causes of high pressures.
- Alarm limits
Trigger
If the trigger is set too high, then the patient may want to breathe but is not strong enough to meet the trigger requirement.
For example, if the trigger is 3L/min then the patient needs to reach this flow rate for the ventilator to deliver a pressure supported breath. However, if they are weak or too sedated then they might not have the strength to generate this flow rate resulting in a breath not being delivered when wanted.
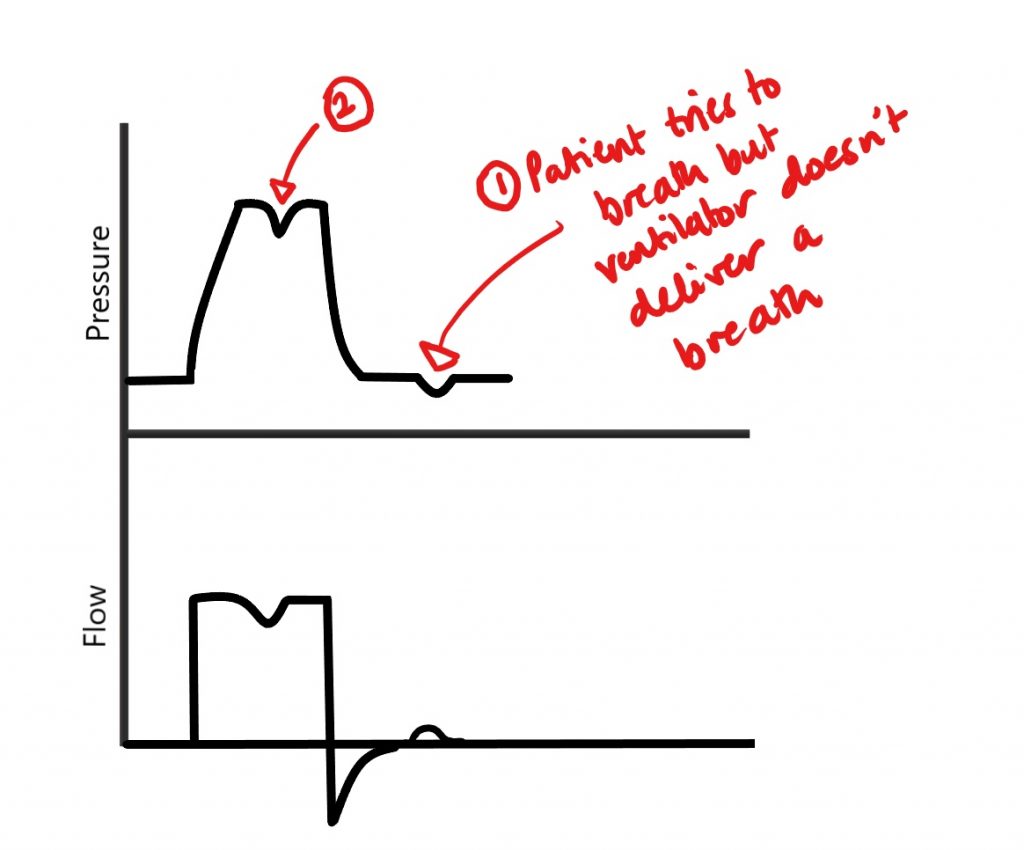
At point 1 the patient tries to breath, but the ventilator does not deliver a breath. If the flow trigger was lower, then this small deflection in flow may be sufficient to trigger the ventilator.
At point 2 the patient tries to breath despite a delivered volume being given and the ventilator transitions to expiration. This may occur in mandatory modes of ventilation so transitioning to a patient triggered mode would be appopriate.
Conversely if the trigger is too low, then the ventilator may mistake some interference (e.g. cardiac oscillations, shivering) as the patient wanting a breath. This will result in the ventilator delivering breaths when the patient does not want them. This will often lead to an elevated respiratory rate.
High levels of intrinsic PEEP can also cause problems triggering as this intrinsic PEEP needs to be overcome prior to the ventilator being triggered.
What to do?
- Review mode – does the patient need to be in a mandatory mode of ventilation?
- Review trigger sensitivity, and increase or decrease as appropriate
- It may also be that the patient is too sedated – reducing sedation (if able) may result in increased strength and drive to trigger the ventilator
- Assess for high levels of intrinsic PEEP
- This is done with an expiratory hold. Some ventilators have a specific “PEEPi” diagnostic manoeuvre.
- Treating this is aimed at prolonging expiration (decreased I-time, decreased respiratory rate) and treating the cause (bronchospasm).
- If not bronchospastic and no evidence of gas trapping on flow waveforms (see below) then increasing applied PEEP may be necessary.
Flow
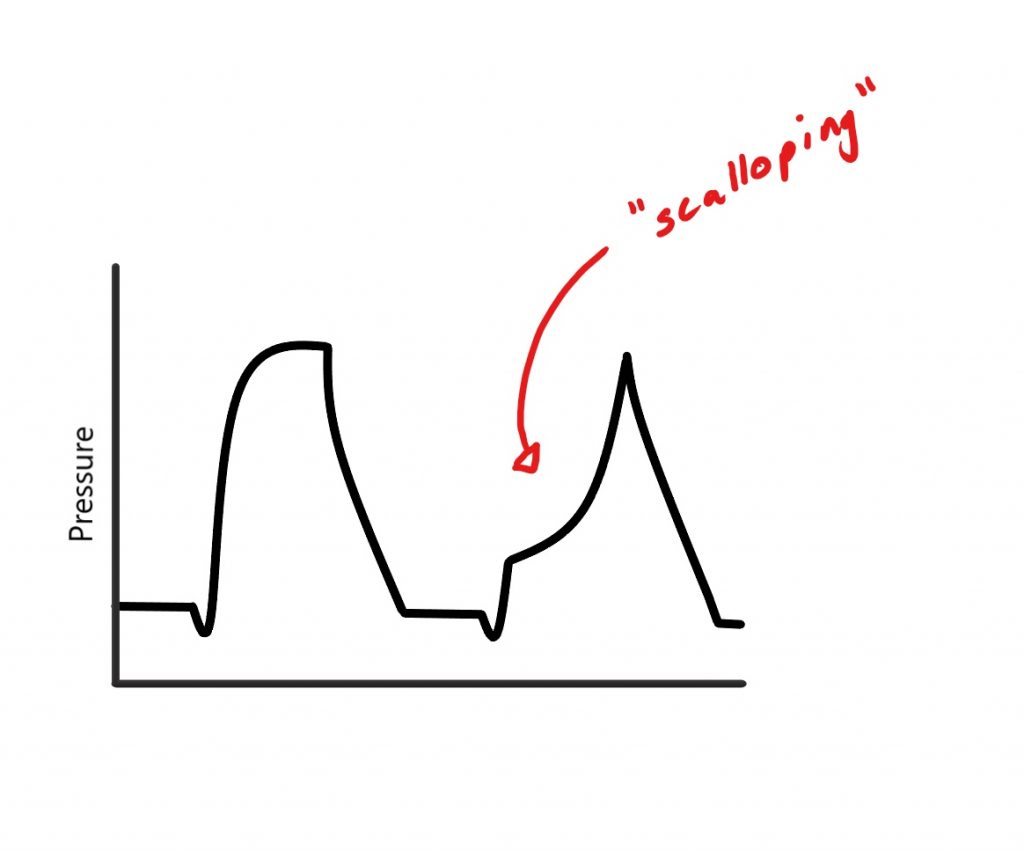
The flow is the rate at which the gas mixture is delivered to the patient. Sometimes if this is too low then the patient may not feel as if they are getting enough of a breath resulting in dyssynchrony.
What to do?
- In volume limited breaths then you can directly increase the flow
- “Autoflow” may need to be turned off
- In pressure supported breaths you could try increasing the pressure support; or decreasing the rise time (this the time taken to reach the set pressure, therefore by decreasing it will result in the set pressure is being reached faster with higher flow rates).
- Increasing flow will increase peak pressures.
Cycling
Cycling is when the ventilator transitions to expiration. Commonly this is time cycled or flow cycled.
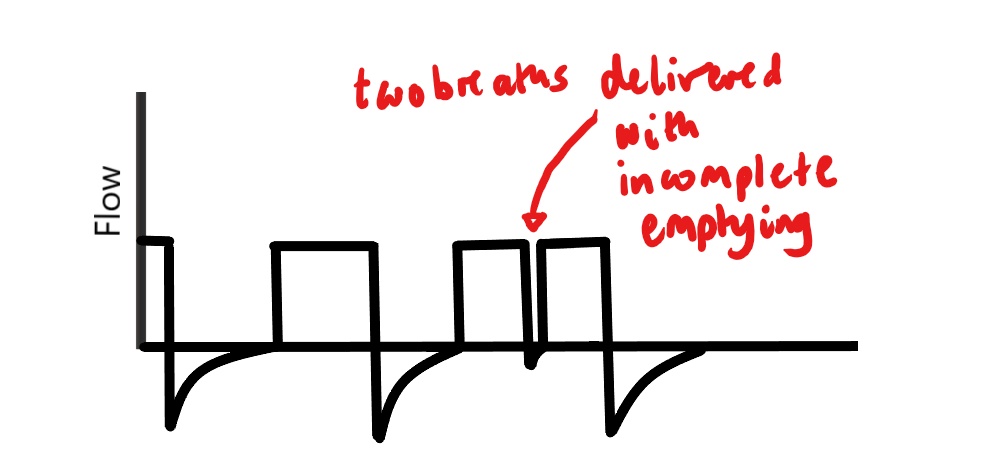
If the ventilator cycles to expiration but the patient still wants to inspire then this can lead to dyssynchrony. This could be caused by the inspiratory time being too short, inspiratory flows being too low or an insufficient tidal volume being delivered. Sometimes “double triggering can occur”. This looks like two breaths in quick succession. This can result in high peak pressures as there has been insufficient for expiration of the first breath.
What to do?
- Aim is to increase delivered tidal volume
- Lengthen inspiratory time
- Reduce the expiratory flow trigger
- The expiratory flow trigger is % of peak expiratory flow that causes the ventilator to cycle to expiration
- For example, if set at 25% then once the expiratory flow falls to 25% of the maximal expiratory flow rates then the ventilator will cycle to expiration.
- Usually this around 25-30%, if this value is decreased then the inspiratory flow will continue for longer resulting in larger tidal volumes.
- The expiratory flow trigger is % of peak expiratory flow that causes the ventilator to cycle to expiration
Other problems seen on waveforms
The ventilator waveform (also known as a scalar) depicts a certain parameter (e.g. volume, pressure or flow) against time (on the x-axis).
Certain problems can be spotted on these waveforms:
Gas Trapping
Gas trapping can be recognised by failure of the expiratory flow reaching zero. This can lead to dynamic hyperinflation.
This occurs when the expiratory time is too short, resulting in the inspired volumes not being fully expired. Mostly commonly causes result from increased expiratory resistance (e.g. bronchospasm, kinked tubing, clogged HME filters). This causes increased intrathoracic volumes and pressures. Increased intrathoracic pressures can lead to reduced venous return and hypotension, as well as increased work to trigger the ventilator.

What to do?
- Treat the cause (e.g. bronchospasm requires bronchodilators)
- Lengthen expiration (reduce respiratory rate, decrease I-time)
- Review PEEP settings
- If profound hypoxia or haemodynamic instability then disconnection from the ventilator can result in the lungs being able to empty
Leaks
Leaks in the ventilator circuit can be seen by failure of the volume scalar to return to zero (i.e. there is loss of some expiratory volume that is not measured by the ventilator). This is eve more noticeable on flow-volume loops.
Leaks in the circuit can result from issues with ventilator, breaks in the circuit or loose connections, or an endotracheal tube cuff leak.
ETT cuff leaks can occur from damage to the cuff (anywhere from the pilot balloon to the inflatable cuff) or a functioning cuff that is not sitting appropriately in the trachea resulting in air leaking around the cuff.

What to do?
- Review cuff pressure (is it less than what was previously recorded?)
- The cuff may need to be re-inflated
- Is a cuff leak audible?
- This sounds like a “gurgling” noise
- What tube size is it?
- Sometimes the cuff on a small tube might not completely occlude the trachea (e.g. if a size 7 was put in an overweight and tall patient)
- Are all connections on the circuit and ventilator tight and can you see any damage to the ventilator tubing?
- Discuss with your senior about advancing the tube 1cm. Sometimes despite being fixed at the teeth the tube can migrate in a cephalad direction.
- Should always prompt senior review as may require a tube exchange.
References and Further Reading
Hamilton Medical: Ventilator Asynchrony Reference Card
Anaesthesiology: Management of Patient – Ventilator Asynchrony
Respiratory Care: Ventilator Graphics: Scalars, Loops, & Secondary Measures
