Non-invasive ventilation is the provision of ventilatory support via a tight-fitting facemask as opposed to an endotracheal tube. As with invasive ventilation, it provides positive pressure ventilation.
There are two main ways in which this pressure is delivered, either continuous positive airway pressure (CPAP) or bi-level positive airway pressure (BiPAP).
CPAP
CPAP provides a continuous level of PEEP (positive end expiratory pressure) throughout the respiratory cycle. This recruits alveoli and prevents alveolar collapse thus improving oxygenation and work of breathing. It is predominantly used for type 1 respiratory failure.
BiPAP
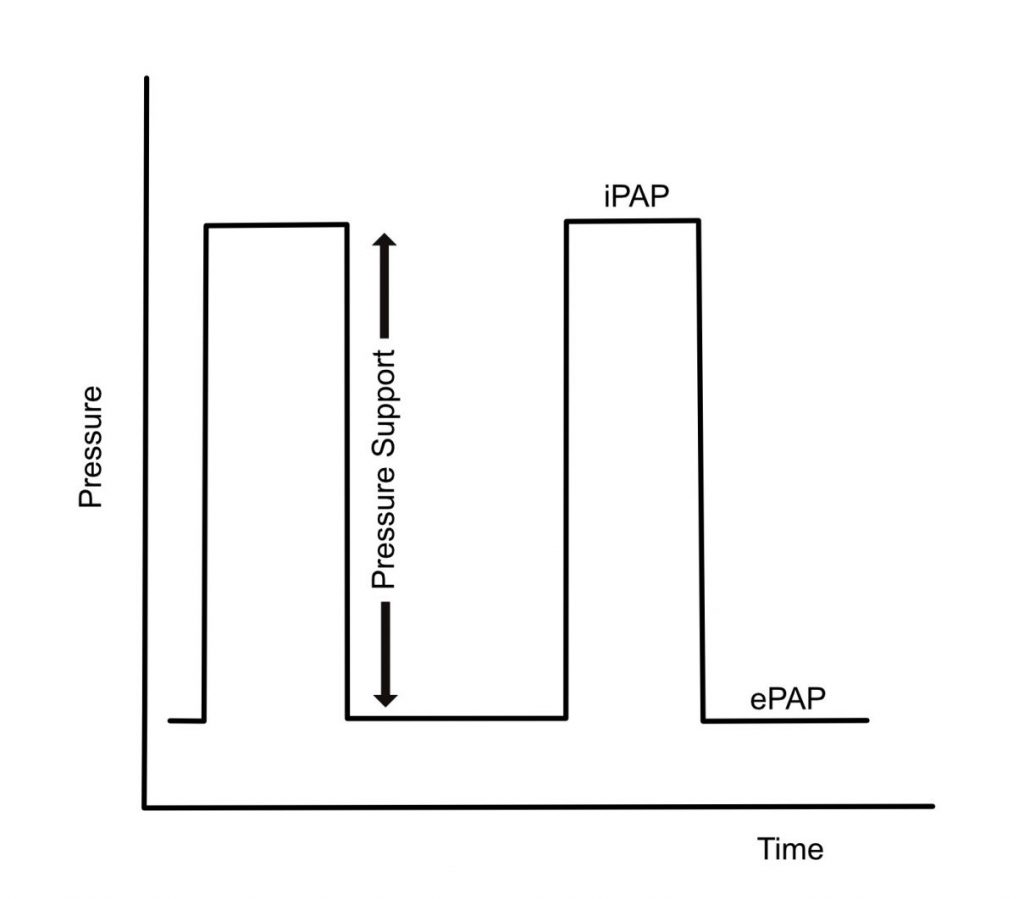
As the name suggests, this mode delivers two levels of pressure: an inspiratory pressure (iPAP) and expiratory pressure (ePAP). ePAP is analogous to PEEP (or the value set in CPAP). BiPAP is used for type 2 respiratory failure, or failure of ventilation.
Set Up and Important Settings
- Patient explanation and reassurance is key. It can be an extremely unpleasant experience and take a period of time to become accustomed to it. Depending on the acuity of the situation, the face mask can just be held on by the patient so they can experience what NIV feels like, prior to the mask being strapped tightly on.
- It is also helpful to establish an action that they can use if they have had enough or can’t tolerate it.
- Ensure an appropriate mask size is selected. If the leak is high once the patient is established on NIV, then the mask and fit will need to be re-evaluated.
- Helmets can also be used as a delivery mechanism. Nasal masks tend to be used for the chronic treatment of OSA.
- FiO2: can start at 1 and wean to SpO2 target
- CPAP: one pressure is set e.g. 5 cm H20.
- BiPAP: two pressures are set:
- Expiratory Pressure (ePAP)
- Inspiratory Pressure (iPAP) or pressure support (which is the amount of pressure delivered above ePAP)
- Start at low pressures e.g. iPAP 10 cm H20 and ePAP 5 cm H2O
- This is referred to as 10/5
- These settings can also be described as an ePAP of 5 cm H2O and a pressure support of 5 cm H2O.
- This is referred to as 10/5
- If needed then gradual increases, in 2cm H2O increments, as tolerated to a maximum of 16/8. Higher pressures may be used but would necessitate senior guidance or use of a local policy.
- Oxygenation can be improved by increasing the ePAP or FiO2
- Ventilation (CO2 removal) can be increased by increasing the PS (or the iPAP relative to the ePAP)
- Increasing from 10/5 to 12/7 doesn’t increase the ventilation provided as the pressure support in both examples is 5 cm H2O. It will improve oxygenation though.
- A back up respiratory rate can also be set.
- Be aware that when starting positive pressure ventilation then hypotension may occur.
- Titrate pressures and FiO2 to clinical state, SpO2 and target ABG parameters.
- A repeat ABG should be done 1 hour following initiation of NIV
- It is important to consider the disease process – a pneumonic process will take longer to resolve and may get worse prior to improvement so clear parameters as to what would define failure of NIV need to be considered at the outset. This would also include a decision as to whether the invasive ventilation would be in the patient’s interest, or if NIV would be the ceiling of respiratory support.
Contraindications
This is not an exhaustive list
- Inability to protect airway e.g. reduced GCS / inability to clear secretions
- Undrained pneumothorax
- Facial Trauma
- Cardiac / Respiratory Arrest
- Significant cardiovascular instability
- Significant vomiting
- In the immediate period post UGI surgery – may require discussion between ICU and surgical team
- Patient intolerance (including severe agitation)/ refusal
High Flow Oxygen
The use of high flow nasal cannula (HNFC) to deliver oxygen has increased rapidly over the last few years. Some of the purported benefits of HFNC include:
- Humidification – this maintains mucociliary function and is more comfortable for the patient
- High FiO2 can be provided at high flow rates – this can decrease work of breathing.
- Provision of PEEP – the exact amount is debated and varies between patient but is thought to be in the realm of 2 – 6 cmH20 (at high flow rates with well-fitting nasal cannula)
- Patient comfort – often much improved compared to NIV
References and Further Reading
Oxford Medical Education: Starting Non-Invasive Ventilation
Rebel EM: High Flow Nasal Cannula (HFNC) – Part 1: How it works
Author: George Walker
